资料与方法
一、对象
二、仪器与方法
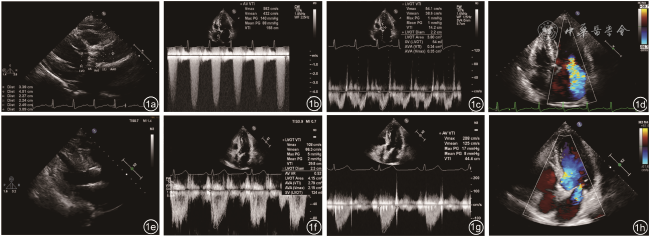
图1 重度主动脉瓣狭窄患者经导管主动脉瓣置换(TAVR)术前与术后6个月随访超声心动图图像。图a~d为术前超声图像,其中图a为胸骨旁左心室长轴切面测量主动脉根部解剖结构,可显示左心室流出道、主动脉瓣环、主动脉窦部、窦管交界处、升主动脉(图中AA为主动脉瓣环,AoS为主动脉窦部,STJ为窦管交界处,AAO为升主动脉);图b,c为心尖五腔心切面勾勒左心室流出道、主动脉瓣口频谱多普勒,获得速度时间积分及主动脉瓣相关参数;图d为心尖五腔心切面彩色多普勒显示重度二尖瓣反流。图e~h为术后6个月超声图像,其中图e为胸骨旁左心室长轴切面显示人工生物主动脉瓣位置固定;图f根据连续方程法估算人工主动脉瓣有效瓣口面积为2.15 cm2;图g示主动脉瓣平均跨瓣压差(AVPGmean)从术前的88 mmHg(1 mmHg=0.133 kPa)降至术后的8 mmHg;图h为彩色多普勒显示重度二尖瓣反流术后转为轻度二尖瓣反流 |
三、统计学分析
结果
一、一般资料及手术情况
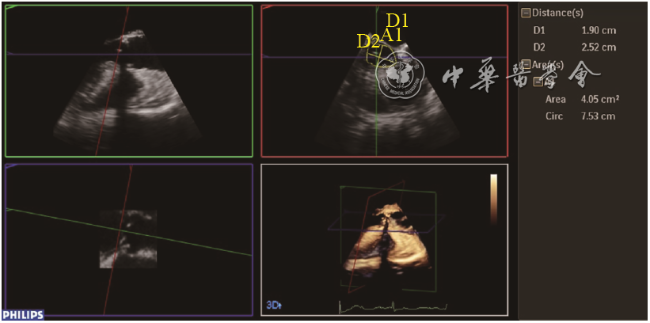
二、3D-TEE与MSCT对术前主动脉根部解剖结构的评估
表1 3D-TEE与MSCT术前评估主动脉根部结构比较( |
| 参数 | 3D-TEE | MSCT | t值 | P值 |
|---|---|---|---|---|
| 主动脉瓣环 | ||||
最大径(cm) | 26.1±2.08 | 26.2±2.4 | -0.12 | 0.901 |
最小径(cm) | 21.2±2.04 | 21.1±2.06 | 0.12 | 0.902 |
面积(cm2) | 425.8±70.23 | 418.5±68.65 | 0.41 | 0.681 |
| AVA(cm2) | 62.3±13.84 | 61.6±18.66 | 0.17 | 0.869 |
注:3D-TEE为三维经食管超声心动图;MSCT为多层螺旋CT;AVA为主动脉瓣有效瓣口面积 |
三、TAVR术前与术后6个月超声心动图参数比较
表2 TAVR术前与术后6个月超声心动图常规参数比较 |
| 参数 | 术前(n=47) | 术后6个月(n=47) | 统计值 | P值 |
|---|---|---|---|---|
| AORD(mm, ±s) | 32.6±4.32 | 32.0±4.53 | t=0.57 | 0.572 |
| LAD(mm, ±s) | 43.9±6.46 | 42.1±7.51 | t=1.23 | 0.226 |
| LVEDD(mm, ±s) | 49.7±7.94 | 46.9±6.14 | t=1.93 | 0.059 |
| LVESD(mm, ±s) | 34.8±9.40 | 30.2±6.11 | t=3.04 | 0.004 |
| IVST(mm, ±s) | 13.3±1.98 | 12.1±1.93 | t=2.72 | 0.009 |
| PWT(mm, ±s) | 12.2±1.24 | 11.1±1.45 | t=4.13 | <0.001 |
| PASP(mmHg, ±s) | 47.3±14.48 | 38.6±8.70 | t=3.27 | 0.002 |
| LVEF(%, ±s) | 57±12.4 | 64±8.3 | t=-3.36 | 0.002 |
| MR中度及以上[例(%)] | 8(17) | 3(6) | χ2=2.57 | 0.109 |
| TR中度及以上[例(%)] | 7(15) | 2(4) | χ2=1.97 | 0.161 |
| AR中度及以上[例(%)] | 14(30) | 0 | χ2=16.45 | <0.001 |
注:1 mmHg=0.133 kPa;TAVR为经导管主动脉瓣置换;AORD为主动脉根部内径;LAD为左心房内径;LVEDD为左心室舒张末期内径;LVESD为左心室收缩末期内径;IVST为室间隔厚度;PWT为左心室后壁厚度;PASP为肺动脉收缩压;LVEF为左心室射血分数;MR为二尖瓣反流;TR为三尖瓣反流;AR为主动脉瓣反流 |
表3 TAVR术前与术后6个月主动脉瓣相关超声心动图参数比较( |
| 参数 | 术前(n=47) | 术后6个月(n=47) | t值 | P值 |
|---|---|---|---|---|
| AVPGmax(mmHg) | 102±31.3 | 21±7.7 | 17.14 | <0.001 |
| AVPGmean(mmHg) | 59±18.5 | 11±4.3 | 16.65 | <0.001 |
| AVA(cm2) | 0.67±0.16 | 1.8±0.24 | -24.50 | <0.001 |
| Vmax(m/s) | 4.96±0.71 | 2.26±0.42 | 21.53 | <0.001 |
注:1 mmHg=0.133 kPa;TAVR为经导管主动脉瓣置换;AVPGmax为主动脉瓣最大跨瓣压差;AVPGmean为主动脉瓣平均跨瓣压差;AVA为主动脉瓣有效瓣口面积;Vmax为主动脉瓣峰值血流速度 |