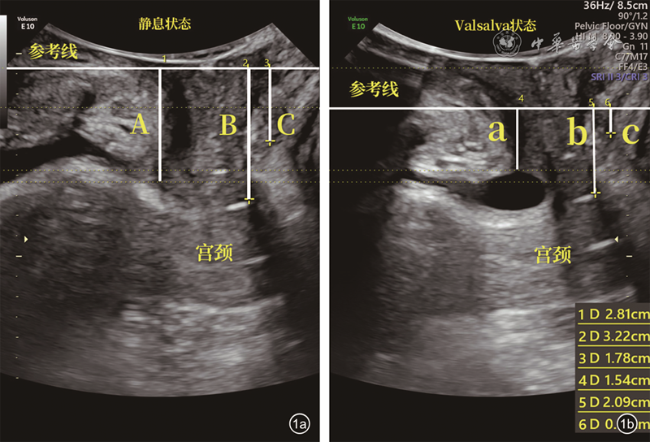
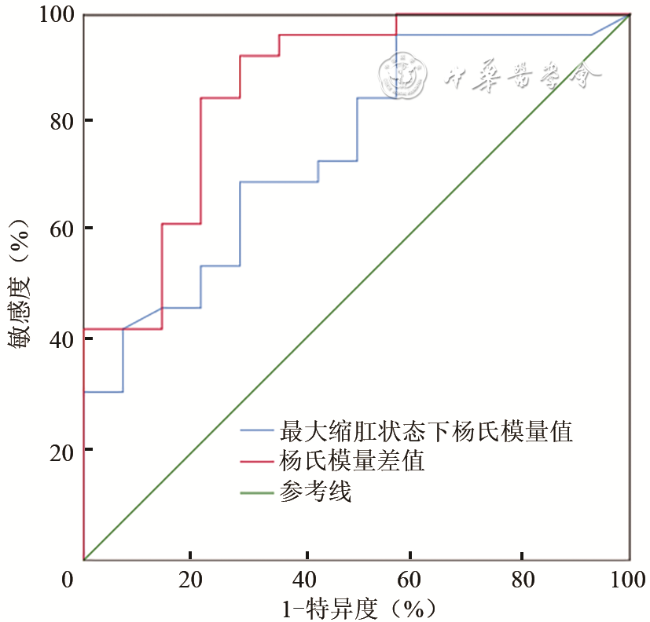
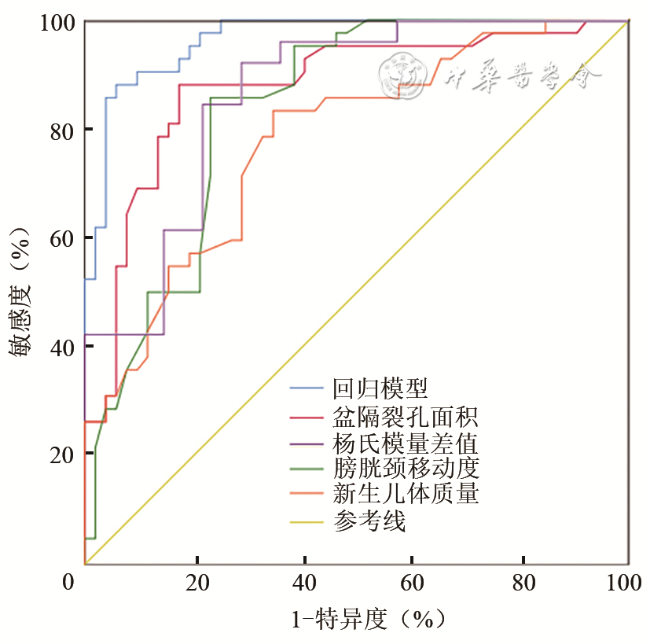
本研究应用单因素分析以及二分类Logistic回归对阴道分娩者产后PFD的相关因素进行综合分析并建立回归模型,包括临床参数、经会阴超声检查参数及杨氏模量值。将单因素分析中对诊断PFD有意义的变量纳入方程,结果显示新生儿体质量、BND和LHA是阴道分娩后PFD的独立危险因素,杨氏模量值差值是阴道分娩后PFD的独立保护因素。本研究中LHA的
OR值为3.328,相对于其他特征变量,是准确性最高的特征参数,在临床工作中应对此予以足够重视,这与Dietz等
[9]的研究结果一致,他们认为PR撕脱伤和LHA的扩张是盆腔脏器脱垂的独立危险因素。王秋静
[10]也发现LHA与产后压力性尿失禁的发生密切相关,均高于其他二维超声诊断参数,
OR值为10.513。有研究发现阴道分娩时,为使胎儿正常通过,孕妇肛提肌可拉长至原来的2.5倍
[11],造成LHA的扩大。本研究还发现杨氏模量值差值是阴道分娩后PFD的独立保护因素,其差值越大,阴道分娩后越不可能出现PFD。Handa等
[12]研究发现肛提肌肌力与盆腔脏器脱垂成反比,肛提肌肌力每增加5 cm H
2O(1 cm H
2O=0.098 kPa),盆腔脏器脱垂发生的
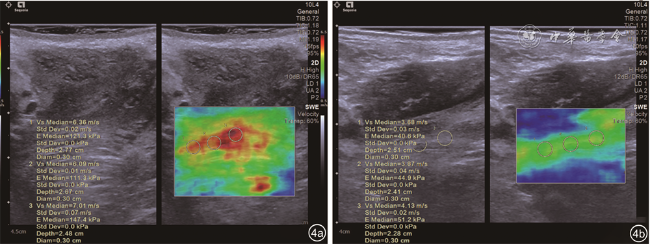
OR值为0.87。牛旺等
[13]在肛提肌弹性成像技术研究中也证实了这点,他们认为PFD患者肛提肌成分中肌小节内结蛋白和波形蛋白表达减低、成纤维细胞增多导致纤维化修复增生,会导致盆底肌肌力及肌张力逐渐减弱,造成主动收缩的杨氏模量值变小,PR成分的改变会造成静息状态下杨氏模量值变大,从而使杨氏模量差值出现差异性。本研究中虽然BND的
OR值较LHA低,但比盆底超声其他二维参数对阴道分娩后PFD的相关性更大。Laterza等
[14]研究发现,阴道分娩后肛提肌损伤的女性1年后仅有泌尿系统的症状而无其他PFD的相关症状,但并未对原因作出过多解释。Nordin和Frankel
[15]研究骨骼肌基本生物力学发现,弹性变形是由外力引起的可逆过程,如不超过阈值,一旦外力不再作用,弹性变形就会回到初始状态,笔者认为PR在最大缩肛状态下,PR的弹性变形对直肠、子宫的活动限制更大,牵拉脏器向腹内侧运动,而膀胱颈部的限制相对较小,从而解释了BND较中后盆腔COD、RAD对阴道分娩后PFD的相关性更大,对阴道分娩后更容易出现泌尿系统症状的原因。新生儿体质量作为阴道分娩后PFD的独立危险因素之一,当新生儿体质量大于3342 g时诊断效能较高,其敏感度和特异度为83.33%和65.38%,这与杨彩霞和唐淑稳
[16]的研究结果一致。