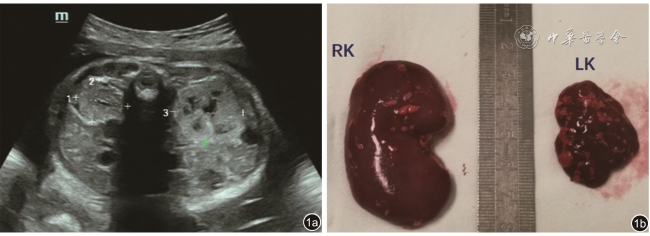
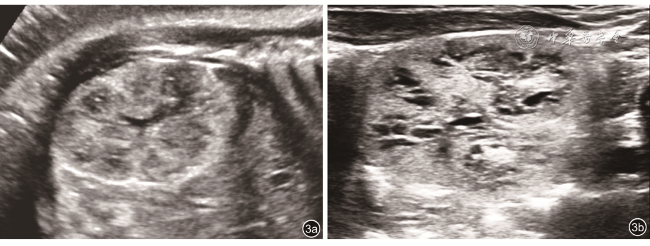
2. 超声诊断方法:所有超声检查先由具有产前筛查资质的超声科医师执行,发现问题后转诊至具有产前诊断资质超声医师。参照国际妇产科超声学会的产科常规超声应用指南,依次对胎儿不同系统器官及胎儿附属物(羊水、胎盘、脐带)进行常规测量。胎儿肾检查内容包括双侧肾大小、形态、皮髓质回声、皮髓质分界、集合系统以及有无囊肿。肾皮质回声高于肝脾回声,诊断为肾回声增强
[1,7]。早中孕期及晚孕期分别采用羊水最大垂直深度(maximum vertical pocket,MVP)或羊水指数(amniotic fluid index,AFI)评价羊水量,羊水量异常超声诊断标准
[8]:MVP≥8 cm或AFI≥25 cm提示羊水过多;MVP≤2 cm或AFI≤5 cm诊断为羊水过少。肾体积异常诊断标准
[9, 10](双侧肾体积明显不一致时,统计归类取远离正常值的肾体积):通过矢状面测量肾长轴,或者计算肾体积(长×宽×厚×
),显著增大为>97
th百分位,显著缩小为<3
th百分位。根据既往研究
[8,11]皮髓质分界清晰定义为正常,皮髓质分界模糊、缺失或者回声倒置定义为异常;将髓质回声低-无回声定义为正常,高回声以及囊性变定义为异常。