资料与方法
一、对象
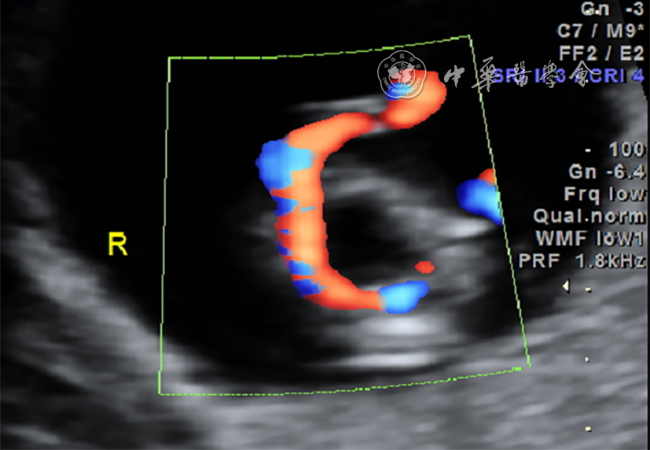
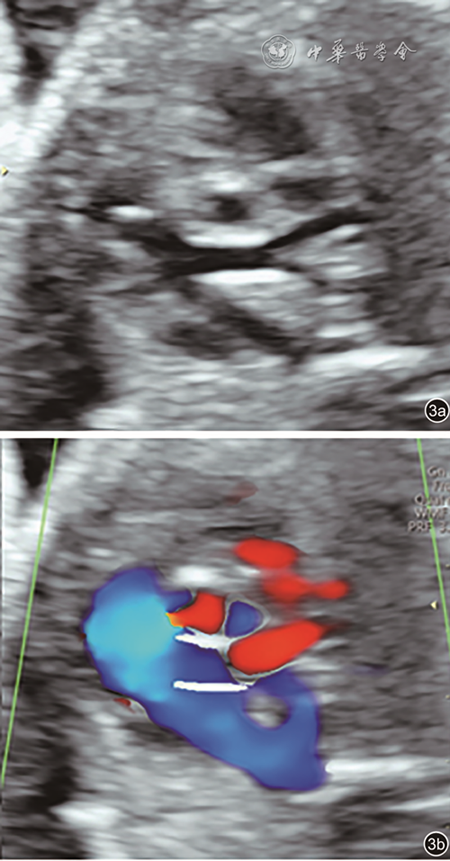
二、仪器与方法
三、单脐动脉胎儿分组及超声软指标
四、纳入标准及排除标准
五、染色体检查
六、统计学分析
结果
一、iSUA和niSUA病例的一般临床资料对比
表1 iSUA及niSUA病例的一般临床资料对比 |
| 项目 | iSUA组(n=202) | niSUA组(n=69) | 统计值 | P值 |
|---|---|---|---|---|
| 孕龄(岁, ±s) | 30.64±4.79 | 30.23±4.24 | t=0.688 | 0.432 |
| 孕次 | χ2=0.0035 | 0.953 | ||
| 1次 | 71 | 24 | ||
| 2次或更多 | 125 | 43 | ||
| 未知 | 6 | 2 | ||
| 有无吸烟史 | χ2=0.0747 | 0.785 | ||
| 有 | 10 | 4 | ||
| 无 | 186 | 63 | ||
| 未知 | 6 | 2 | ||
| 受孕方式 | χ2=0.0317 | 0.859 | ||
| 自然受孕 | 177 | 61 | ||
| 辅助生殖 | 19 | 6 | ||
| 未知 | 6 | 2 | ||
| 有无不良孕产史 | χ2=0.0227 | 0.880 | ||
| 有 | 8 | 3 | ||
| 无 | 154 | 52 | ||
| 未知 | 40 | 14 |
注:iSUA为孤立型单脐动脉,niSUA为非孤立型单脐动脉;统计检验剔除了未知病例 |
二、niSUA组胎儿的结构异常分布
三、入组单脐动脉病例的染色体异常统计及结果分布
表2 各组单脐动脉胎儿染色体结果异常分布情况 |
| 分组 | 获得染色体结果(例) | 染色体异常[例(%)] | 染色体异常种类 |
|---|---|---|---|
| iSUA | 202 | 4(1.98) | 5号、10号染色体微重复各1例,6号染色体微缺失1例,4号、21号染色体倒位1例 |
| niSUA合并软指标异常 | 17 | 1(5.88) | 7q11.23微重复综合征1例 |
| niSUA合并单一畸形 | 35 | 4(11.43) | 1号染色体微重复1例,15号染色体约有50%的比例重复一个拷贝数1例,18号染色体数目3/2条1例,9号或11号染色体异常(具体不详)1例 |
| niSUA合并多发畸形 | 17 | 4(23.53) | 13号染色体数目3条1例,Rubinstein-Taybi综合征Ⅰ型相关基因CREBBP存在一处杂合突变1例,2号、4号染色体微缺失各1例 |
注:各组染色体异常发生率比较,差异具有统计学意义(χ2=19.99,P=0.002);iSUA为孤立型单脐动脉,niSUA为非孤立型单脐动脉 |