资料与方法
一、对象
二、仪器与方法
三、统计学分析
结果
一、一般临床资料比较
表1 各组研究对象一般临床资料比较( |
| 组别 | 例数 | 年龄(岁) | 孕前BMI(kg/m2) | 分娩前BMI(kg/m2) | 产后BMI(kg/m2) | 新生儿体质量(kg) |
|---|---|---|---|---|---|---|
| SVD组 | 50 | 33±3.66 | 21.40±2.25 | 26.49±2.21 | 23.47±1.82 | 3.41±0.43 |
| FVD组 | 150 | 29±3.48a | 21.11±2.36 | 26.13±2.51 | 22.99±2.39 | 3.33±0.37 |
| CS组 | 50 | 28±3.75b | 20.92±2.62 | 26.30±2.30 | 22.82±2.02 | 3.43±0.56 |
| 对照组 | 120 | 23±2.97c | - | - | - | - |
| F值 | 124.68 | 0.52 | 0.44 | 1.22 | 1.37 | |
| P值 | <0.001 | 0.598 | 0.645 | 0.297 | 0.257 |
注:BMI为体质量指数,SVD为二次经阴道分娩组,FVD为初次经阴道分娩组,CS为剖宫产组;a与SVD组比较,差异具有统计学意义(t=6.95,P<0.001),b与SVD组比较,差异具有统计学意义(t=6.75,P<0.001),c与SVD组比较,差异具有统计学意义(t=18.64,P<0.001),a与c比较,差异具有统计学意义(t=15.01,P<0.001),b与c比较,差异具有统计学意义(t=9.23,P<0.001);-表示无数据 |
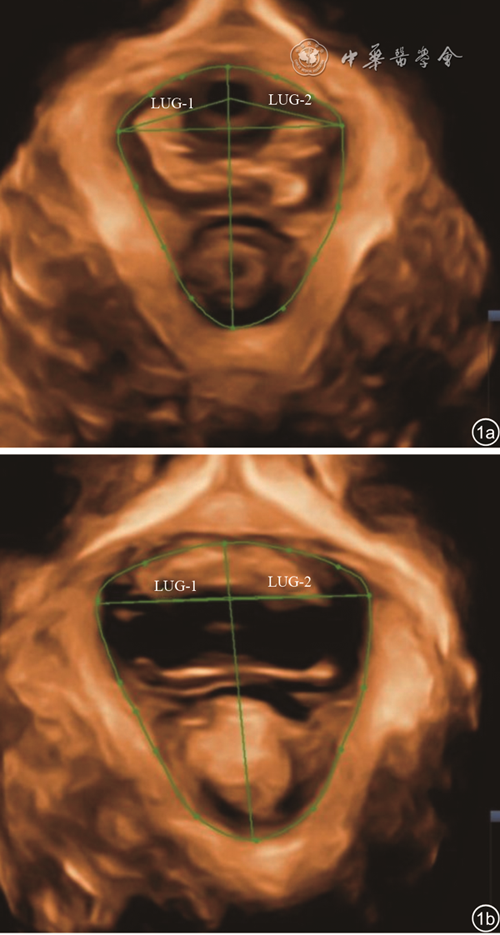
二、各组间静息状态及最大Valsalva状态下LH面积比较
表2 各组研究对象间肛提肌裂孔面积测值比较( |
| 组别 | 例数 | 静息状态 | Valsalva状态 | t值 | P值 |
|---|---|---|---|---|---|
| SVD组 | 50 | 16.59±3.12 | 22.80±8.37 | 4.92 | <0.001 |
| FVD组 | 150 | 15.34±3.50a | 18.46±6.63a | 5.10 | <0.001 |
| CS组 | 50 | 13.09±2.78b | 15.58±3.91b | 3.67 | <0.001 |
| 对照组 | 120 | 11.09±2.47c | 13.11±5.30c | 3.78 | <0.001 |
| F值 | 31.89 | 11.14 | |||
| P值 | <0.001 | <0.001 |
注:SVD为二次经阴道分娩组,FVD为初次经阴道分娩组,CS为剖宫产组;a与SVD组比较,差异具有统计学意义(t=2.25、3.74,P=0.026、<0.001),b与SVD组比较,差异具有统计学意义(t=5.92、5.53,P均<0.001),c与SVD组比较,差异具有统计学意义(t=12.21、9.07,P均<0.001),a与b比较,差异具有统计学意义(t=4.13、2.91,P<0.001、=0.004),a与c比较,差异具有统计学意义(t=11.25、7.19,P均<0.001),b与c比较,差异具有统计学意义(t=4.63、2.97,P<0.001、=0.003) |
三、POP组和无POP组间比较
表3 POP组与无POP组间肛提肌裂孔面积比较( |
| 组别 | 例数 | 静息状态 | Valsalva状态 |
|---|---|---|---|
| 无POP组 | 203 | 12.38±2.17 | 15.59±3.50 |
| POP组 | 167 | 14.88±3.49 | 20.93±6.53 |
| t值 | 8.06 | 9.50 | |
| P值 | <0.001 | <0.001 |
注:POP为盆底器官脱垂 |