资料与方法
一、对象
二、仪器与方法
三、统计学分析
结果
一、一般临床资料
表1 不同性别分组一般资料比较结果( |
| 组别 | 人数 | 年龄(岁) | 身高(m) | 体质量(kg) | 体质量指数 |
|---|---|---|---|---|---|
| 男性组 | 48 | 37.42±8.72 | 1.73±0.07 | 72.84±11.23 | 24.43±2.92 |
| 女性组 | 43 | 37.19±9.32 | 1.63±0.06 | 56.20±7.99 | 21.28±2.75 |
| t值 | -0.122 | -7.290 | -8.056 | -5.282 | |
| P值 | 0.903 | <0.001 | <0.001 | <0.001 |
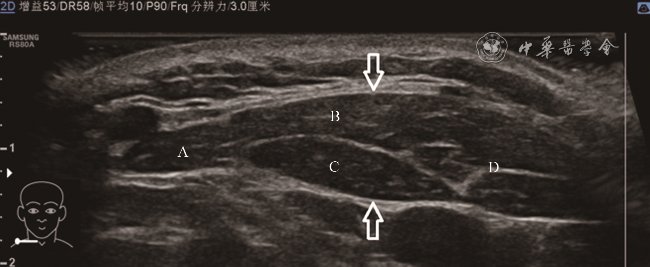
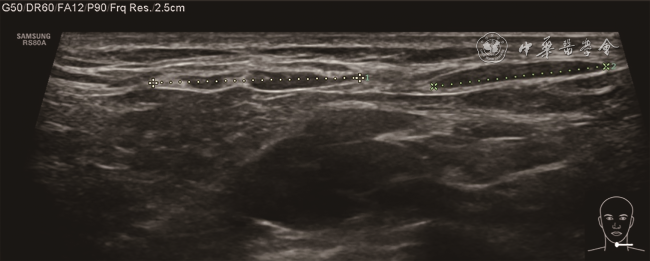
二、正常胸锁乳突肌的超声形态及变异
三、正常胸锁乳突肌的测值
表2 健康志愿者双侧胸锁乳突肌总厚度及4个部分厚度测量值比较(cm, |
| 组别 | 人数 | 胸锁乳突肌总厚度 | 乳突锁骨束厚度 | 乳突胸骨束厚度 | 枕骨锁骨束厚度 | 枕骨胸骨束厚度 |
|---|---|---|---|---|---|---|
| 左侧组 | 91 | 0.91±0.16 | 0.53±0.13 | 0.68±0.14a | 0.39±0.10a,b | 0.29±0.09a,b,c |
| 右侧组 | 91 | 0.89±0.17 | 0.54±0.13 | 0.68±0.14a | 0.41±0.10a,b | 0.27±0.09a,b,c |
| t值 | 0.595 | -0.699 | -0.079 | -0.973 | 1.197 | |
| P值 | 0.552 | 0.485 | 0.937 | 0.332 | 0.233 |
注:a与乳突锁骨束厚度比较,b与乳突胸骨束厚度比较,c与枕骨锁骨束厚度比较,差异均具有统计学意义(P均<0.001) |
表3 不同性别健康志愿者胸锁乳突肌总厚度及4个部分厚度测量值比较(cm, |
| 组别 | 人数 | 胸锁乳突肌总厚度 | 乳突锁骨束厚度 | 乳突胸骨束厚度 | 枕骨锁骨束厚度 | 枕骨胸骨束厚度 |
|---|---|---|---|---|---|---|
| 男性组 | 48 | 0.98±0.15 | 0.60±0.12 | 0.74±0.14 | 0.44±0.11 | 0.29±0.08 |
| 女性组 | 43 | 0.81±0.12 | 0.46±0.08 | 0.62±0.11 | 0.36±0.07 | 0.26±0.10 |
| t值 | -8.366 | -9.529 | -6.772 | -6.430 | -2.558 | |
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | 0.011 |
表4 健康志愿者双侧胸锁乳突肌内部结构测量平均值(cm, |
| 项目 | 左侧组 | 右侧组 | t值 | P值 |
|---|---|---|---|---|
| 锁骨束止点宽度 | 3.05±0.71 | 3.13±0.71 | -0.759 | 0.449 |
| 锁骨束腱膜宽度 | 0.84±0.48 | 0.81±0.47 | 0.485 | 0.628 |
| 锁骨束腱膜厚度 | 0.08±0.03 | 0.08±0.04 | 0.140 | 0.889 |
| 胸骨束止点宽度 | 0.86±0.15 | 0.88±0.14 | -0.763 | 0.446 |
| 胸骨束腱膜宽度 | 0.69±0.23 | 0.74±0.24 | 1.249 | 0.213 |
| 胸骨束腱膜厚度 | 0.12±0.06 | 0.13±0.06 | 0.609 | 0.543 |
| 锁骨束腱膜长度 | 2.82±0.99 | 2.65±0.93 | 1.183 | 0.238 |
| 胸骨束腱膜长度 | 7.17±1.46 | 7.45±1.55 | -1.251 | 0.212 |
表5 不同性别健康志愿者胸锁乳突肌内部结构测量平均值(cm, |
| 项目 | 男性组 | 女性组 | t值 | P值 |
|---|---|---|---|---|
| 锁骨束止点宽度 | 3.27±0.67 | 2.89±0.70 | 3.740 | 0.000 |
| 锁骨束腱膜宽度 | 0.93±0.49 | 0.71±0.43 | 3.149 | 0.002 |
| 锁骨束腱膜厚度 | 0.09±0.04 | 0.08±0.03 | 1.331 | 0.185 |
| 胸骨束止点宽度 | 0.91±0.15 | 0.82±0.12 | 4.481 | 0.000 |
| 胸骨束腱膜宽度 | 0.78±0.25 | 0.64±0.20 | 4.102 | 0.000 |
| 胸骨束腱膜厚度 | 0.13±0.06 | 0.12±0.06 | 0.715 | 0.475 |
| 锁骨束腱膜长度 | 2.95±0.92 | 2.50±0.95 | 3.243 | 0.001 |
| 胸骨束腱膜长度 | 7.35±1.47 | 7.26±1.55 | 0.366 | 0.714 |