20世纪80年代,McGoon指数(McGoon index,MGI)和肺动脉指数(pulmonary artery index,PAI)又称Nakata指数开始用于评估先天性心脏病(congenital heart disease,CHD)患者的肺血管发育
[1-2],MGI被认为是评价肺血管床整体发育的指标。临床上,MGI常与Nakata指数共同作为法洛四联症(tetralogy of Fallot,TOF)一期根治手术最重要的手术指征,在TOF患者术前评估、术式选择及术后干预方面提供了重要的参考依据,与患者预后密切相关
[3]。Hiraishi等
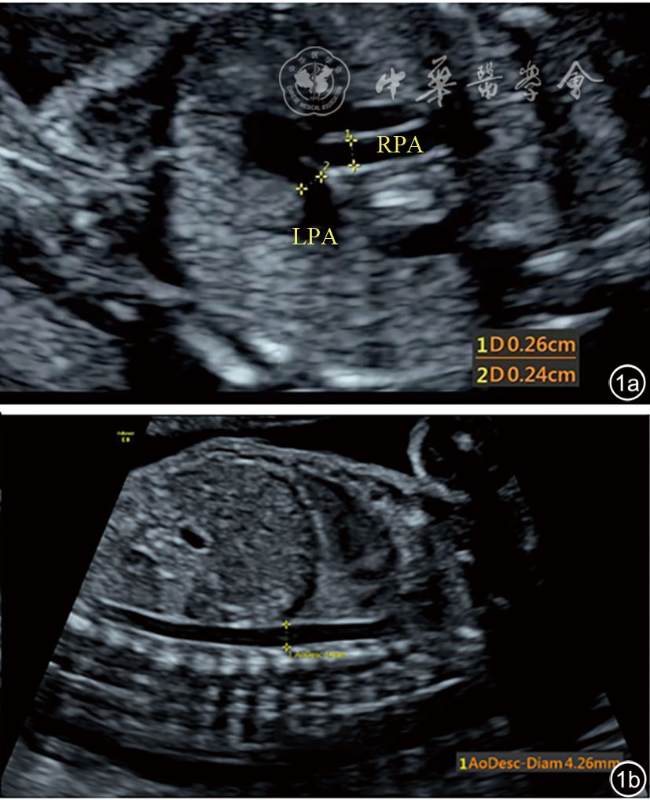
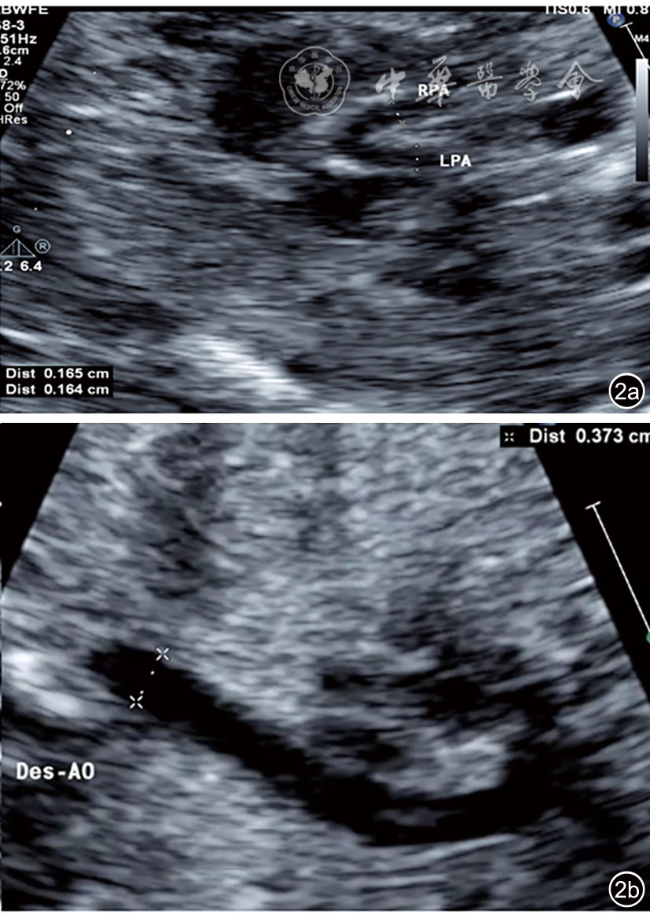
[4]应用心血管造影与超声心动图分别测量主肺动脉(main pulmonary artery,MPA)、右肺动脉(right pulmonary artery,RPA)、左肺动脉(left pulmonary artery,LPA)的近端、中端、远端内径以及肺动脉狭窄处内径,发现超声与心血管造影测值高度相关,提示超声测量的MGI可以较准确地评估肺动脉的发育程度,指导手术方式的选择。过去MGI主要用于成人或儿童CHD患者的评估,但胎儿时期血流动力学及肺发育情况与出生后截然不同,近些年已有对胎儿MGI的研究报道。郭勇等
[5]对TOF胎儿的研究显示,MGI明显低于正常胎儿,提示此类CHD在胎儿时期可能已经对肺动脉发育产生一定不良影响。同时发现RPA和LPA内径之和与胎儿肺体积呈明显的线性正相关,提示二维超声测量左右肺动脉一定程度上可反映胎儿肺发育情况。本文将进一步探讨不同孕龄正常胎儿的MGI变化情况及在不同肺血流量状态下的多种类型CHD胎儿MGI的差异,并探索其临床应用价值。
 表示,所有资料经正态性检验及方差齐性检验,正常对照组内4个亚组之间的比较及正常对照组与病例组间的比较均采用单因素方差分析,进一步多重比较分析采用LSD-t法。以P<0.05为差异有统计学意义。
表示,所有资料经正态性检验及方差齐性检验,正常对照组内4个亚组之间的比较及正常对照组与病例组间的比较均采用单因素方差分析,进一步多重比较分析采用LSD-t法。以P<0.05为差异有统计学意义。
 )
)