资料与方法
一、对象
二、仪器与方法
三、统计学分析
 表示,2组间比较采用独立样本t检验;组内各段动脉参数比较采用单因素方差分析,进一步两两比较采用S-N-K检验。以P<0.05为差异有统计学意义。
表示,2组间比较采用独立样本t检验;组内各段动脉参数比较采用单因素方差分析,进一步两两比较采用S-N-K检验。以P<0.05为差异有统计学意义。结果
一、一般资料
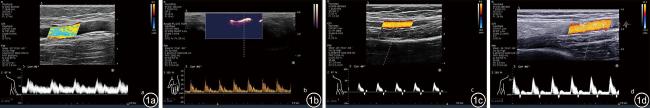
二、2组间动脉血流频谱形态比较
表1 造瘘侧上肢动脉与健康成人上肢动脉血流频谱波形占比[例(%)] |
| 动脉波形 | BA | UA | RA | UPPDA | RPPDA |
|---|---|---|---|---|---|
| 造瘘侧上肢(n=81) | |||||
| 单相波 | 81(100) | 81(100) | 81(100) | 81(100) | 81(100) |
| 非单相波 | |||||
| 典型三相波 | 0 | 0 | 0 | 0 | 0 |
| 非典型三相波 | 0 | 0 | 0 | 0 | 0 |
| 健康上肢(n=103) | |||||
| 单相波 | 49(47.57) | 93(90.30)a | 89(86.41)a | 103(100)abc | 102(99.03)abc |
| 非单相波 | |||||
| 典型三相波 | 34(33.01) | 5(4.85) | 6(5.82) | 0 | 1(0.97) |
| 非典型三相波 | 20(19.42) | 5(4.85) | 8(7.77) | 0 | 0 |
注:BA为肱动脉;UA为尺动脉;RA为桡动脉;UPPDA为尺侧指掌侧固有动脉;RPPDA为桡侧指掌侧固有动脉;与BA相比,aP<0.05;与UA相比,bP<0.05;与RA相比,cP<0.05 |
三、2组间动脉超声参数对比
表2 造瘘侧上肢与健康成人上肢动脉血流动力学参数( |
| 动脉 | 内径(mm) | PSV(cm/s) | MDV(cm/s) | EDV(cm/s) | RI | Slope(cm/s2) | V-Flow(ml/min) |
|---|---|---|---|---|---|---|---|
| 造瘘侧上肢(n=81) | |||||||
| BA | 6.24±0.99* | 133.29±48.08* | 59.18±22.02* | 63.33±24.42* | 0.53±0.10* | 641.91±370.00* | 875.69±462.05* |
| UA | 2.52±0.61*a | 107.32±42.68*a | 47.65±30.61*a | 50.51±32.10*a | 0.58±0.18* | 649.57±315.79* | 121.28±101.91*a |
| RA | 2.85±0.86*ab | 104.90±63.31*a | 54.19±40.94* | 56.66±40.63* | 0.53±0.23* | 411.39±335.73*ab | 172.73±158.85*a |
| UPPDA | 0.76±0.23*abc | 26.78±14.60abc | 7.67±5.57*abc | 7.91±5.64*abc | 0.74±0.13*abc | 200.30±170.49abc | 2.67±2.07*abc |
| RPPDA | 0.76±0.29*abc | 17.46±9.41*abc | 5.27±3.73*abc | 5.37±3.81*abc | 0.73±0.13*abcd | 107.46±87.30*abcd | 2.20±1.32*abc |
| F值 | 685.15 | 131.17 | 78.87 | 89.08 | 34.40 | 64.27 | 214.47 |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
| 健康上肢(n=103) | |||||||
| BA | 3.72±0.65 | 74.01±17.47 | 6.95±6.89 | 7.63±7.10 | 0.90±0.09 | 787.20±239.05 | 68.44±31.85 |
| UA | 1.85±0.38a | 65.43±15.57a | 13.56±9.38a | 14.50±9.32a | 0.79±0.10a | 601.12±150.38a | 31.61±26.63a |
| RA | 2.09±0.30ab | 58.09±14.02ab | 11.90±7.34a | 12.64±7.48a | 0.79±0.10a | 541.57±152.53ab | 29.53±18.44a |
| UPPDA | 0.93±0.14abc | 30.05±15.95abc | 11.17±8.03ab | 11.56±6.28ab | 0.64±0.11abc | 182.31±86.51abc | 4.88±3.89abc |
| RPPDA | 0.86±0.14abc | 24.99±12.37abcd | 8.67±5.96bcd | 8.91±6.03bcd | 0.66±0.11abc | 153.20±86.18abc | 3.42±2.76abc |
| F值 | 991.18 | 210.59 | 12.35 | 13.34 | 105.07 | 223.57 | 172.09 |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
注:PSV为收缩期峰值速度;MDV为舒张期平均速度;EDV为舒张末期速度;RI为阻力指数;Slope为收缩期峰值血流加速度;V-Flow为血流容积;BA为肱动脉;UA为尺动脉;RA为桡动脉;UPPDA为尺侧指掌侧固有动脉;RPPDA为桡侧指掌侧固有动脉;组内比较:与BA比较,aP<0.05;与组内UA比较,bP<0.05;与组内RA比较,cP<0.05;与组内UPPDA比较,dP<0.05;组间比较:与健康成人同名动脉参数比较,*P<0.05 |

 )
)