资料与方法
一、对象
二、仪器与方法
1.仪器:
2.二维超声及UGAP检查:
3.临床资料收集及分组:
三、统计学分析
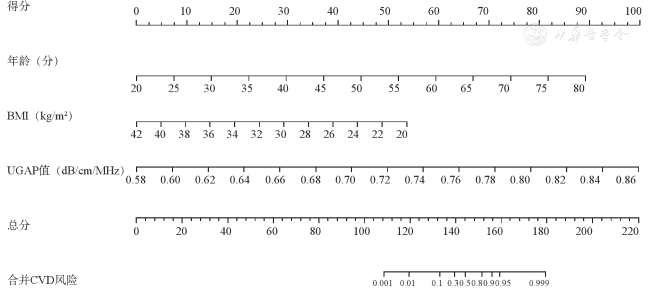
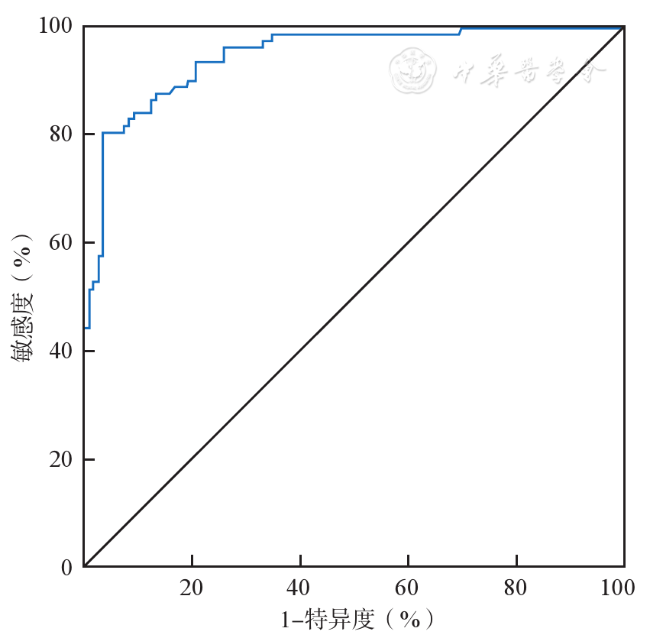
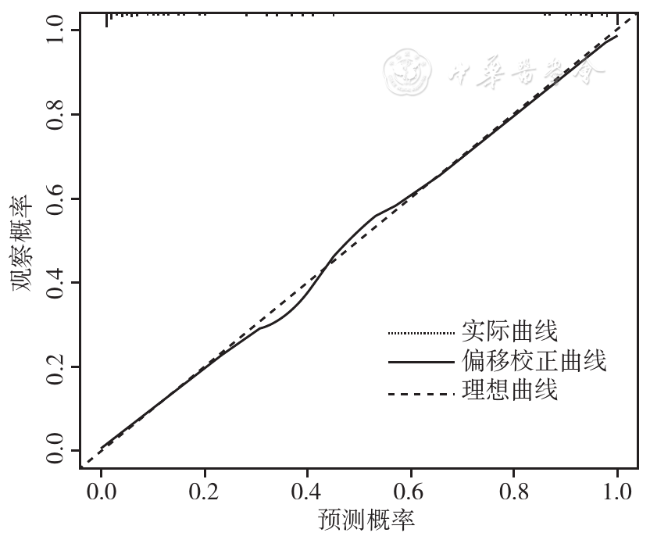
 ±s表示,2组间比较采用独立样本t检验。非正态分布的数据,以M(P25,P75)表示,2组间比较采用非参数检验。计数资料以例(%)表示,2组间比较采用χ2检验。应用单因素和多因素线性回归分析各变量与UGAP值之间的关联。将单因素分析中P<0.05的变量纳入多因素回归分析,确定UGAP值的独立影响因素。此外,采用Spearman等级相关来评估UGAP值与肝脂肪变性二维超声诊断分级之间的相关性;采用Kruskal-Wallis检验比较不同程度肝脂肪变性的UGAP值差异。受试者间UGAP值的一致性通过计算组内相关系数(intraclass correlation coefficient,ICC)来评估。采用Logistic回归和Nomogram模型分析NAFLD患者并发CVD的危险因素,并应用ROC曲线及校正曲线评估该模型的临床效能。P<0.05为差异具有统计学意义。
±s表示,2组间比较采用独立样本t检验。非正态分布的数据,以M(P25,P75)表示,2组间比较采用非参数检验。计数资料以例(%)表示,2组间比较采用χ2检验。应用单因素和多因素线性回归分析各变量与UGAP值之间的关联。将单因素分析中P<0.05的变量纳入多因素回归分析,确定UGAP值的独立影响因素。此外,采用Spearman等级相关来评估UGAP值与肝脂肪变性二维超声诊断分级之间的相关性;采用Kruskal-Wallis检验比较不同程度肝脂肪变性的UGAP值差异。受试者间UGAP值的一致性通过计算组内相关系数(intraclass correlation coefficient,ICC)来评估。采用Logistic回归和Nomogram模型分析NAFLD患者并发CVD的危险因素,并应用ROC曲线及校正曲线评估该模型的临床效能。P<0.05为差异具有统计学意义。结果
一、一般资料
表1 NAFLD组与对照组一般临床资料比较[M(P25,P75)] |
| 临床资料 | 对照组(n=73) | NAFLD组(n=204) | 统计值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 56.5(47,64) | 56(50,63) | Z=-0.035 | 0.972 |
| BMI(kg/m2) | 22.75(21.85,23.55) | 26.90(25.6,27.7) | Z=-11.490 | <0.001 |
| SLD(cm) | 2.19(1.75,2.42) | 2.13(1.88,2.36) | Z=-0.094 | 0.925 |
| ALT(U/L) | 22.75(18.1,27.15) | 50.50(44.7,60.05) | Z=-11.339 | <0.001 |
| AST(U/L) | 22.95(18.35,26.7) | 53.60(44.15,65.2) | Z=-11.234 | <0.001 |
| GGT(U/L) | 58.55(34.2,86.05) | 63.40(35.9,87.15) | Z=-0.363 | 0.717 |
| Glu(mmol/L) | 5.08(4.67,5.62) | 5.91(5.63,7.06) | Z=-7.595 | <0.001 |
| TC(mmol/L) | 3.75(3.21,4.15) | 5.26(4.98,5.86) | Z=-12.564 | <0.001 |
| TG(mmol/L) | 1.16(0.94,1.35) | 2.28(1.89,2.69) | Z=-12.746 | <0.001 |
| HDL(mmol/L) | 1.21(0.88,1.36) | 1.04(0.92,1.17) | Z=-2.425 | 0.015 |
| LDL(mmol/L) | 3.06(2.32,3.69) | 3.09(2.82,3.63) | Z=-0.492 | 0.623 |
TP(g/L, ±s) ±s) | 67.00±5.75 | 68.02±5.99 | t =-1.264 | 0.207 |
| AKP(U/L) | 73.8(60.2,89.75) | 73.4(64.05,87.8) | Z=-0.788 | 0.431 |
| UGAP-1(dm/cm/MHz) | 0.61(0.59,0.62) | 0.71(0.68,0.74) | Z=-11.498 | <0.001 |
| UGAP-2(dm/cm/MHz) | 0.62(0.6,0.63) | 0.72(0.69,0.76) | Z=-11.462 | <0.001 |
注:BMI为体质量指数;SLD为皮肤-肝包膜距离;ALT为丙氨酸氨基转移酶;AST为门冬氨酸氨基转移酶;GGT为γ-谷氨酰转移酶;Glu为血糖;TC为总胆固醇;TG为甘油三酯;HDL为高密度脂蛋白;LDL为低密度脂蛋白;TP为总蛋白;AKP为碱性磷酸酶;UGAP-1、UGAP-2分别为2位检查医师测量的超声引导衰减参数;NAFLD为非酒精性脂肪性肝病 |
二、与UGAP相关的影响因素分析
表2 影响NAFLD患者UGAP值的单因素线性回归分析 |
| 因素 | 非标准化系数 | 标准化系数 | t值 | P值 | R2 | 调整R2 | F(P)值 | |
|---|---|---|---|---|---|---|---|---|
| B | 标准误 | Beta | ||||||
| 年龄 | 0 | 0 | 0.043 | 0.708 | 0.479 | 0.002 | -0.002 | 0.502(0.479) |
| BMI | 0.022 | 0 | 0.936 | 44.099 | <0.001 | 0.876 | 0.876 | 1944.6395(<0.001) |
| SLD | 0.001 | 0.012 | 0.006 | 0.099 | 0.921 | 0 | -0.004 | 0.01(0.921) |
| ALT | 0.004 | 0 | 0.971 | 67.354 | <0.001 | 0.943 | 0.943 | 4536.536(<0.001) |
| AST | 0.002 | 0 | 0.841 | 25.778 | <0.001 | 0.708 | 0.707 | 664.486(<0.001) |
| GGT | 0 | 0 | 0.059 | 0.98 | 0.328 | 0.003 | 0 | 0.96(0.328) |
| Glu | 0.026 | 0.002 | 0.583 | 11.887 | <0.001 | 0.339 | 0.337 | 141.308(<0.001) |
| TC | 0.068 | 0.001 | 0.955 | 53.408 | <0.001 | 0.912 | 0.912 | 2852.434(<0.001) |
| TG | 0.079 | 0.001 | 0.959 | 55.858 | <0.001 | 0.919 | 0.919 | 3120.156(<0.001) |
| HDL | -0.029 | 0.018 | -0.098 | -1.633 | 0.104 | 0.01 | 0.006 | 2.666(0.104) |
| LDL | -0.009 | 0.005 | -0.106 | -1.763 | 0.079 | 0.011 | 0.008 | 3.109(0.079) |
| TP | 0.001 | 0.001 | 0.11 | 1.832 | 0.068 | 0.012 | 0.008 | 3.357(0.068) |
| AKP | 0 | 0 | 0.062 | 1.025 | 0.306 | 0.004 | 0 | 1.051(0.306) |
| 肝脂肪变性程度 | 0.064 | 0.002 | 0.908 | 35.842 | <0.001 | 0.824 | 0.823 | 1284.649(<0.001) |
注:BMI为体质量指数;SLD为皮肤-肝包膜距离;ALT为丙氨酸氨基转移酶;AST为门冬氨酸氨基转移酶;GGT为γ-谷氨酰转移酶;Glu为血糖;TC为总胆固醇;TG为甘油三酯;HDL为高密度脂蛋白;LDL为低密度脂蛋白;TP为总蛋白;AKP为碱性磷酸酶;UGAP为超声引导衰减参数;NAFLD为非酒精性脂肪性肝病 |
表3 影响NAFLD患者UGAP值的多因素线性回归分析 |
| 因素 | 非标准化系数 | 标准化系数 | t值 | P值 | VIF | R2 | 调整R2 | F(P)值 | |
|---|---|---|---|---|---|---|---|---|---|
| B | 标准误 | Beta | |||||||
| 常数 | 0.387 | 0.011 | 35.057 | <0.001 | - | 0.976 | 0.976 | 1841.781(<0.001) | |
| BMI | 4.0×10-3 | 0.001 | 0.190 | 7.691 | <0.001 | 6.906 | |||
| AST | 5.75×10-5 | 0 | 0.024 | 1.330 | 0.185 | 3.652 | |||
| Glu | 0 | 0.001 | -0.006 | -0.465 | 0.643 | 1.600 | |||
| TC | 0.024 | 0.002 | 0.332 | 13.265 | <0.001 | 7.112 | |||
| TG | 0.028 | 0.002 | 0.339 | 11.959 | <0.001 | 9.081 | |||
| 肝脂肪变性程度 | 0.011 | 0.001 | 0.153 | 7.463 | <0.001 | 4.774 | |||
注:BMI为体质量指数;AST为门冬氨酸氨基转移酶;Glu为血糖;TC为总胆固醇;TG为甘油三酯;UGAP为超声引导衰减参数;NAFLD为非酒精性脂肪性肝病 |
三、UGAP技术评价肝脂肪变性的可行性分析
表4 UGAP值的操作者间一致性分析 |
| 参数 | 组内相关系数 | 95%CI | P值 |
|---|---|---|---|
| 总体 | 0.977 | 0.972~0.982 | <0.001 |
| 肝脂肪变性诊断分级 | |||
| S0 | 0.885 | 0.823~0.926 | <0.001 |
| S1 | 0.851 | 0.779~0.901 | <0.001 |
| S2 | 0.887 | 0.832~0.925 | <0.001 |
| S3 | 0.909 | 0.827~0.953 | <0.001 |
注:UGAP为超声引导衰减参数 |
四、NAFLD合并CVD组与未合并CVD组患者的基线资料比较
表5 NAFLD合并CVD组与未合并CVD组患者的基线资料比较[M(P25,P75)] |
| 资料 | NAFLD合并CVD组(n=83) | NAFLD未合并CVD组(n=121) | 统计值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 62(57,66) | 52(46,58) | Z=-7.269 | <0.001 |
| BMI(kg/m2) | 27.6(26.7,29.6) | 26.3(25.1,27.2) | Z=-6.223 | <0.001 |
| 收缩压(mmHg) | 130(130,140) | 125(120,140) | Z=-3.846 | <0.001 |
| 舒张压(mmHg) | 85(80,90) | 83(80,90) | Z=-0.364 | 0.715 |
| UGAP(dm/cm/MHz) | 0.76(0.71,0.81) | 0.69(0.68,0.72) | Z=-7.483 | <0.001 |
| TC(mmol/L) | 4.95(4.15,5.51) | 5.14(4.78,5.63) | Z=-1.903 | 0.057 |
| TG(mmol/L) | 1.94(1.53,2.44) | 2.01(1.48,2.53) | Z=-0.464 | 0.643 |
HDL(mmol/L, ±s) ±s) | 1.05±0.20 | 1.06±0.21 | t =0.242 | 0.809 |
| LDL(mmol/L) | 3.13(2.32,3.66) | 3.07(2.89,3.58) | Z=-0.744 | 0.457 |
| Glu(mmol/L) | 6.39(5.86,7.99) | 5.78(5.43,6.09) | Z=-6.00 | <0.001 |
| 性别[例(%)] | χ2=0.915 | 0.339 | ||
| 男性 | 41(37.6) | 68(62.4) | ||
| 女性 | 42(44.2) | 53(55.8) | ||
| 吸烟[例(%)] | χ2=17.043 | <0.001 | ||
| 否 | 32(28.1) | 82(71.9) | ||
| 是 | 51(56.7) | 39(43.3) |
注:1 mmHg=0.133 kPa;BMI为体质量指数;UGAP为超声引导衰减参数;TC为总胆固醇;TG为甘油三酯;HDL为高密度脂蛋白;LDL为低密度脂蛋白;Glu为血糖;NAFLD为非酒精性脂肪性肝病;CVD为心血管疾病 |
五、NAFLD合并CVD的多因素逐步Logistic影响因素分析
表6 NAFLD合并CVD的多因素逐步Logistic回归分析 |
| 因素 | B | 标准误差 | Wald χ2值 | P值 | OR值 | 95%CI |
|---|---|---|---|---|---|---|
| 年龄 | 0.29 | 0.047 | 38.2 | <0.001 | 1.337 | 1.219~1.466 |
| BMI | -0.473 | 0.205 | 5.321 | 0.021 | 0.623 | 0.417~0.931 |
| UGAP | 69.919 | 13.449 | 27.027 | <0.001 | 2.32×1030 | 8.27×1018~6.51×1041 |
| 常量 | -54.662 | 8.212 | 44.31 | <0.001 | 0 |
注:BMI身体质量指数;UGAP为超声引导衰减参数 |